Children’s posture control develops from 0-8 years, and there are many important milestones along the way. It is very important that the milestones are achieved.
It is not widely known that at 8 years of age postural reference frames are fully developed. The postural reference frame is the basic muscle pattern that the brain uses to control posture and produce movement, for example, normal walking, or walking pattern problems such as pigeon toes (in-toeing), tip toeing, turned out feet (out-toeing).
The brain references balance to the feet (base of support). If there is something wrong with the structure and/ or alignment of the feet, this affects the process of postural development.
There are many important milestones along the way in the process of postural development, including development of feedforward posture control mechanisms that appear at around 2.5 years. Feed forward postural control mechanisms are based on what the brain has learnt in the first 2 years about which muscle patterns work to control posture, and the brain then begins to anticipate what muscle to use. This means that the muscle patterns begin to become formalised at around 2.5 years of age.
The brain uses sensory information from sections of the nervous system (proprioceptive system, visual system and vestibular system) to plan and pattern muscle contraction/ relaxation sequences in order to develop, organise and control posture.
The normal muscle pattern relies on the brain receiving normal sensory information.
If the information from one system is incorrect/ unclear, then the brain cannot use the normal muscle pattern to control posture, and therefore will use a compensatory muscle pattern, such as pigeon toed walking, tip toe walking, out-turned feet, which may result in constant tripping.
Between 4.5 years and 6 years, the brain weights and integrates sensory information from the proprioceptive system, visual system and vestibular system. If the sensory information from one or more of these systems is not clear or correct, then the brain cannot integrate the information. This results in inefficient muscle patterning, and is seen as delayed or inefficient gross motor skill development.
If the muscle patterns are incorrect, growth will not change them. To change muscle patterns, we must change the sensory information the brain is receiving from the weight bearing joints and muscles themselves. This is what Dr Henry Netscher does at Footlink Kidsfeet.
The development of the Feed-forward posture control mechanisms & Postural reference frames determine what muscles your child uses to control and produce movement.
For example, in children with joint hypermobility (over elastic ligaments that bind bones together to form joints) the joints are unstable and can move in directions that they should not move in. Therefore the proprioceptive system information is not clear and accurate. Because of this the brain will use muscles to do the work of the ligaments … to stabilise the joints.
This means that some muscles are doing extra work and the muscles that produce the opposite action at a joint are under-working. This leads to an imbalance in strength between opposing groups of muscles. This leads to visible alignment problems at joints when the child is walking/ standing/ crawling. These imbalances in opposing muscle groups cause muscles tiredness, aches, pains, and problems with posture control including gross motor skill development.
Commonly, muscle aches in children is thought to be ‘Growing pains’. There are no such things as ‘growing pains’.
Normal growth is not painful. If there is pain, there will be a reason for it, and it its very important to identify the reason.
If the child reports the pain, it is important that the pain is investigated if it persists for more than 2 days.
Sadly, many children are left in pain for 2 years before their parents/ guardians present them to a health professional.
Continued pain causes children to withdraw from physical activity, and sometimes causes self-esteem problems because the child cannot recruit the correct muscle patterns in order to perform a movement task correctly. Therefore they don’t feel successful.
Dr Henry Netscher – click for Resumé
Dr Henry Netscher is the only Podiatrist in Australasia with a PhD (Doctor of Philosophy) on the effects of joint hypermobility on posture control in children. Dr Netscher was a Health and Physical Education teacher prior to being a Podiatrist. His knowledge of sporting activities and the gross motor skills involved in physical activities adds another dimension to his patient management plans.
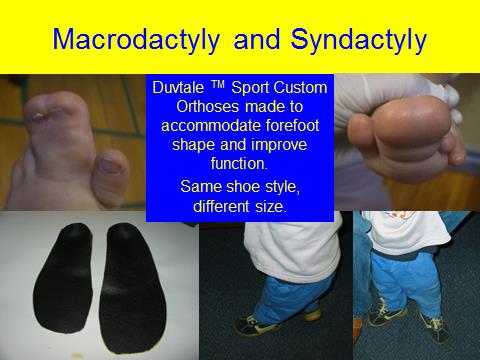
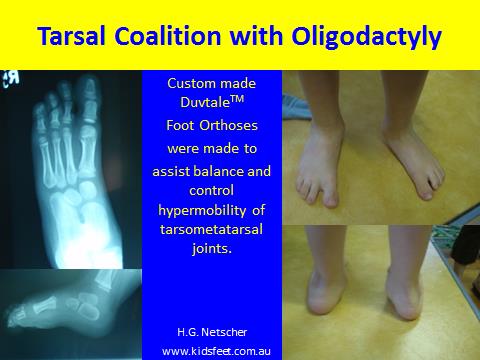
Dr Netscher designed the Duvtale orthotic device specifically to treat balance control problems in children with joint hypermobility.
Dr Netscher has also designed various splints to treat resting alignment disorders in children, including metatarsus adductus (pigeon toes), pseudo-malleolar in-torsion (bowed legs), juvenile hallux valgus (bunions), high/ low-riding toes (crooked toes), talipes calcaneo-valgus (foot stuck up against front of leg), tip-toe walker’s resting alignment.
Things You Need To Know
Commonly, muscle aches in children is thought to be ‘Growing pains’. There are no such things as ‘growing pains’.
Normal growth is not painful. If there is pain, there will be a reason for it, which must be diagnosed.
If the child reports the pain, it is important that the pain is investigated if it persists for more than 2 days.
Sadly, many children are left in pain for 2 years before their parents/ guardians present them to a health professional.
Continued pain causes children to withdraw from physical activity, and sometimes causes self-esteem problems because the child cannot recruit the correct muscle patterns in order to perform a movement task correctly. Therefore they don’t feel successful.
A child cannot grow out of a condition that has a genetic basis. There earlier we assess the child, the better and quicker the improvement.
The arch of the foot does not develop spontaneously at 5 or 6. The arch of the foot is present from birth. The arch is generally covered in fat in small children. Some people find it difficult to distinguish between a fat foot and a flat foot. It is the bony alignment that is the issue in a flat foot. A simple test you can perform at home is to look at the arch of the foot when the child is not weight bearing, and feel for the bones on the inside of the arch. You will feel that the arch is present. Then, have the child stand on the foot. If the bones depress in the mid-region of the foot, then the child has a functional flat foot, which should be assessed.
Muscle weakness does not cause flat feet. Flat feet are generally a sign of joint hypermobility. If the foot looks normal at rest (an arch is present) and flattens (to some extent) during weight bearing, this is an indication that the child has joint hypermobility. Another clue that the child has joint hypermobility is that the toes (2-5) are clawed as the child takes a step and the big toe is up-turned at the end. These feet require early intervention.
Things You Need To Know
- The younger the child the easier and shorter the treatment in general.
- If you think something is wrong with your child’s feet, then it is likely that there is something wrong.
- Don’t wait for your child to grow out of foot problems, because many do not.
- If your child is going to grow out of their foot problems, you should notice steady and gradual improvement from week to week.
- Critical aspect of postural development occur from birth to eight years when the adult gait patterns are formed.
- There are no such things as growing pains. If you think your child has growing pains make an appointment. There will be a reason for the pain.
- The arch of the foot does not develop spontaneously at 5 or 6. If a health professional tells you this, seek another opinion.
You Should Contact Us When
- You first notice a problem with your child’s feet, even if your child is new to the world.
- You think your child has ‘growing pains’, or someone else tells you this.
- A relative, friend, teacher or stranger makes comment about your child’s feet.
- Your child complains of tired or sore feet or legs.
- Your child is not walking by the age of 15 months.
- Your child wants to be carried most of the time.
- Your child falls over often, and often falls over nothing.
- Your child crawls in any way other than on the hands and knees.
- Your child has had surgery on, or broken a bone in, the hip, thigh, knee, shin, ankle, foot.
We Treat
- Gait (walking) related disorders.
- In-toeing. pigeon toes, metatarsus adductus, talipes equino varus
- Out-toeing, talipes calcaneo valgus, peroneus tertuis contracture
- Tip- toe walking
- Delayed walking
- Flat feet
- Limb length differences
- Low muscle tone
- Balance problems and clumsiness
- Sports injuries, including heel pain in athletic children (commonly called Sever’s Disease- this is a misnomer)
- Alignment disorders
- Metatarsus Adductus
- Talipes equino-varus
- Talipes calcaneo-valgus
- Tip-toe walking
- Crooked toes
- Bowed legs
- Bunions
- Tarsal coalition.
- Twisted toes, polydactyly (more than 5 toes per foot), oligodactyly (less than 5 toes per foot), syndactyly (joined together toes), macrodactyly (very large toes).
- Skin conditions
- warts
- corns
- calluses.